Imagine you just launched your tech startup, the office buzzes with fresh ideas, but you keep hearing the same worry: “How am I going to keep my team healthy without blowing our budget?” That feeling of uncertainty is all too common.
The good news is that group health insurance for startups isn’t a luxury reserved for Fortune 500s; it’s a realistic tool that can attract talent, lower turnover, and actually save you money in the long run.
Take Maya’s four‑person app studio in Austin. She thought a health plan would cost more than her monthly cloud bill, but after shopping around she discovered a plan that fit her 2‑50 employee range and slashed her hiring costs by about 15% because candidates started asking, “Do you offer health benefits?”
So how do you replicate Maya’s success? First, map out your headcount and projected growth for the next 12‑18 months. Knowing whether you’ll stay under 10 employees or scale to 30 changes the pool of carriers you can negotiate with.
Next, gather a few quotes. You don’t need to call every insurer; many carriers let you request estimates online in minutes. Compare premium rates, deductibles, and the network of doctors. A quick spreadsheet can turn a vague feeling into a concrete decision.
Don’t forget the hidden perks. Some plans bundle telemedicine, mental‑health apps, and even wellness stipends—features that resonate with a generation that values flexibility. When you bundle these, the overall cost per employee can drop dramatically, turning a perceived expense into a competitive advantage.
If you’re still unsure which plan fits, our guide on group health insurance for small and mid‑size businesses walks you through the most common options, from HMO to PPO, and shows how to align them with your cash flow.
Finally, measure the impact. After you’ve rolled out coverage, use an employee‑experience platform to see how satisfaction scores shift. Tools like Benchmarcx let you benchmark your benefits against industry standards, so you know whether the investment is paying off.
Ready to take the next step? Start gathering quotes today, compare the numbers, and watch your startup’s culture strengthen while your payroll stays under control.
TL;DR
Group health insurance for startups lets you attract top talent, lower turnover, and keep medical costs predictable without draining your cash flow while staying compliant with regulations.
Start gathering quotes today, compare premiums and perks, and use simple tools to measure employee satisfaction, turning benefits into a competitive advantage today.
Understanding the Basics of Group Health Insurance for Startups
So you’ve mapped your headcount, you’ve collected a few quotes, and now you’re staring at the term “group health insurance for startups” and wondering what the heck it actually means. Trust me, you’re not alone. The jargon can feel like a maze, but the core idea is simple: you pool your employees together so the insurer can spread risk and give you a better rate than you’d get buying individual plans.
At its heart, a group plan is a contract between you, the employer, and the carrier. The carrier agrees to cover a defined set of medical services for every eligible employee, and you agree to pay a per‑person premium. Because the risk is shared across the whole team, insurers can negotiate lower prices, especially when you stay under the 50‑employee threshold that many carriers treat as a small‑business sweet spot.
Key components you need to know
First, the eligibility rule. Most carriers require a minimum of two full‑time equivalents (FTEs) to qualify for a group plan. If you’re a solo founder, you’ll need to wait until you hire that second teammate or explore a solo‑owner health exchange.
Second, the type of plan. The most common options are:
- HMO – lower premiums, tighter network, must pick a primary care doctor.
- PPO – higher premiums, broader network, you can see specialists without referrals.
- POS – a hybrid of HMO and PPO.
Which one feels right depends on your team’s preferences. If your engineers love the flexibility of seeing any specialist, a PPO might be worth the extra cost. If your crew is cost‑sensitive and lives near a strong provider network, an HMO could save you a lot.
Third, the cost drivers. Premiums are influenced by:
- Average age of your workforce.
- Geographic location – urban areas tend to be pricier.
- Plan design – deductibles, co‑pays, out‑of‑pocket caps.
- Employer contribution level – many startups cover 70‑80% of the premium to stay competitive.
And here’s a tip: you don’t have to stick with a static contribution. Some startups use a tiered approach where newer hires get a higher subsidy for the first year, then it tapers off as they settle in.
Now, let’s talk about compliance. The Affordable Care Act (ACA) requires applicable large employers (ALEs) – those with 50 or more full‑time equivalents – to offer affordable coverage. Below that threshold, you’re not legally bound, but offering coverage can still be a game‑changer for talent acquisition.
But how do you know if your new health plan is actually moving the needle? That’s where data comes in. By tracking employee satisfaction and health‑care utilization, you can fine‑tune your benefits mix. Benchmarcx provides real‑time benchmarking tools that let you compare your benefits experience against industry standards, so you can see whether your health plan is a win‑win or just another line‑item.
Automation can also take a huge load off your plate. Managing enrollment, tracking eligibility changes, and handling claims can quickly become a part‑time HR job. Assistaix offers AI‑driven automation that can streamline benefits administration, from sending out open‑enrollment reminders to updating payroll deductions automatically.
When you combine smart data with automation, you free up time to focus on what matters: building culture and product. And speaking of culture, remember that health insurance isn’t just a paycheck deduction. It’s a signal that you care about your people’s well‑being.
For a deeper dive into the specific options that work best for startups, check out our guide on group health insurance for small & mid‑size businesses. It breaks down the nuances of each plan type and shows you how to align them with cash‑flow realities.
Below is a quick video that walks you through the enrollment timeline step‑by‑step, so you can visualize the process before you dive in.
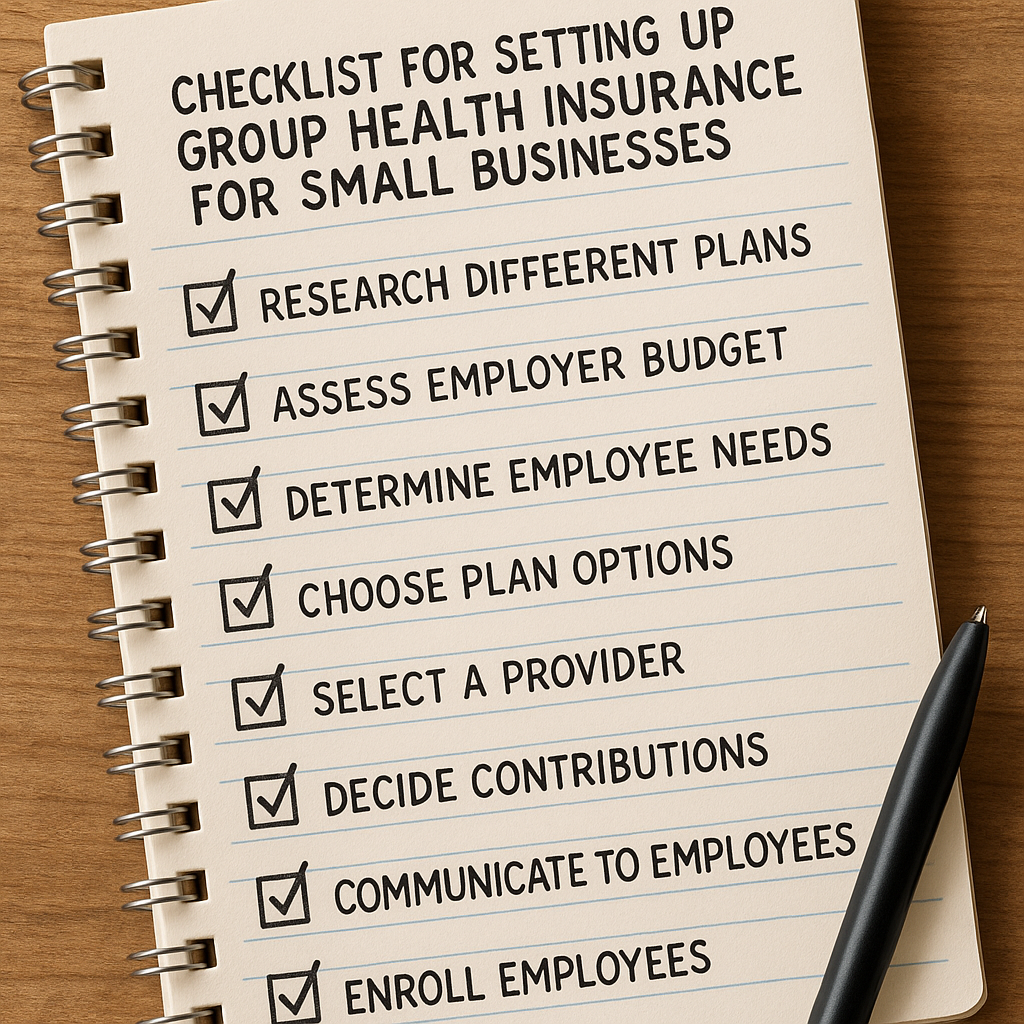
Once you’ve watched the video, you might be wondering what the next concrete move looks like. Here’s a simple checklist you can copy‑paste into your favorite note app:
- Confirm you have at least two FTEs.
- Determine your budget‑friendly contribution percentage.
- Select a plan type (HMO, PPO, POS) that matches your team’s needs.
- Gather at least three quotes from reputable carriers.
- Run the numbers through a benchmarking tool like Benchmarcx.
- Set up an automated enrollment workflow with Assistaix or a similar platform.
\n
Finally, keep the conversation alive. Benefits aren’t a set‑and‑forget item; they evolve as your team grows. Schedule a quarterly “benefits pulse” meeting, ask for candid feedback, and adjust the plan or contribution level accordingly.

By demystifying the basics, you’ve turned a vague worry into a clear roadmap. The next step? Put the plan into motion, watch your talent pool expand, and enjoy the peace of mind that comes with knowing your people are covered.
How to Choose the Right Provider for Your Startup
Alright, you’ve gathered the data, spoken to a broker, and drafted a policy. Now comes the part that feels a bit like dating: picking the right insurance provider. It’s okay to feel a little nervous—after all, this partner will be handling your team’s health for years to come.
1. Pinpoint what matters most to your crew
Start with a quick poll or a short Slack thread. Ask your engineers if they value low premiums, your designers if they need a wide mental‑health network, and your sales folks if telemedicine is a must‑have. Jot down the top three must‑haves.
Typical priorities for startups include:
- Affordable employee contribution (often <9.96% of household income is considered affordable under the ACA)1.
- Broad provider network in the cities where you hire.
- Extra perks like wellness apps or prescription‑drug discounts.
2. Verify the carrier’s small‑group credentials
Not every big insurer offers a true “small‑group” product. Look for language like “small‑group” or “SHOP” in their brochure. If the plan is only listed for 50+ employees, walk away—that’s not a startup‑friendly option.
Check the state’s Department of Insurance website for any complaints or licensing issues. A clean record saves you headaches later.
3. Compare network breadth, not just headline price
It’s tempting to pick the cheapest quote, but ask yourself: can your new hire in Austin actually see a dermatologist within 15 minutes?
Pull a sample of the provider list and search for the clinics your team already trusts.
Most carriers will give you a “network lookup” tool. If you can’t find it online, ask the sales rep to walk you through it on a screen share.
4. Crunch the numbers with a realistic contribution model
Take the premium you’ll pay for a baseline plan and decide how much of it you’ll cover. Many startups start at 60 % and bump it up as cash flow improves. Use a simple spreadsheet:
- Base premium per employee.
- Employer contribution %.
- Employee out‑of‑pocket cost.
- Total monthly cost to the business.
If the total exceeds your budget, look for defined‑contribution HRA options—those let you set a fixed dollar amount and let employees pick the plan that fits them.
5. Hunt for startup‑specific discounts or bundles
Some carriers advertise “new‑company” discounts, especially if you sign up for a multi‑year contract. Others bundle telehealth, mental‑health apps, or even a wellness stipend into the plan at no extra cost.
Ask directly: “Do you have any startup‑friendly add‑ons that won’t blow our runway?” The answer is often a surprised “yes,” because insurers love to lock in fast‑growing teams.
6. Test the provider’s customer service
Before you sign, call the support line and ask a “what‑if” scenario—like a claim for a pre‑existing condition or a request for a referral. Time the hold, note the tone, and see if the rep can walk you through the process without putting you on hold for 20 minutes.
Good service feels like a friendly neighbor: they answer quickly, they’re honest about limitations, and they follow up with an email recap.
7. Run a final checklist
Grab a piece of paper (or a digital note) and tick off these items:
- Provider offers a true small‑group plan.
- Network includes at least 3 doctors in each city you operate.
- Employer contribution fits your budget.
- Any startup‑specific discounts are documented.
- Customer‑service test was satisfactory.
If anything feels shaky, keep looking. The right partner will check all the boxes and still leave room for a quick “let’s talk” call when you have a question.
Bottom line: choosing a provider isn’t a one‑time decision, it’s an ongoing relationship. Re‑evaluate every 12‑18 months, especially after a hiring surge or a change in cash flow. When you treat your health‑insurance partner like a teammate, you’ll keep your startup healthy, happy, and ready to scale.
Comparing Plan Types: HMO, PPO, and POS
Alright, you’ve narrowed down a few carriers and now you’re staring at three acronyms that feel like secret code: HMO, PPO, and POS. Before you get lost in the jargon, let’s break them down in plain English so you can see how each one actually plays out for a startup that’s trying to stretch every dollar.
What’s the real difference?
In a nutshell, an HMO (Health Maintenance Organization) locks you into a network of doctors and usually forces you to get a referral from a primary‑care provider (PCP) before you see a specialist. A PPO (Preferred Provider Organization) gives you a big network to choose from, but you can also go out‑of‑network – you’ll just pay more. A POS (Point‑of‑Service) sits somewhere in the middle: you have a PCP and need referrals for specialists, yet you still get some out‑of‑network coverage, albeit at a higher cost.
UHC explains the nuances of each plan type, noting that POS plans “require referrals to see specialists” and blend features of both HMO and PPO modelsUHC explains the differences between HMO, PPO, and POS plans.
Real‑world startup snapshots
Imagine Maya’s four‑person app studio in Austin. She chose an HMO because the premium was 15 % lower than the PPO options she saw, and her team already trusted a local clinic that was in‑network. The trade‑off? When a developer needed a dermatologist, Maya had to ask the PCP for a referral, adding a day or two to the process. For a tiny team, the cost savings outweighed the extra admin.
Now think about a remote‑first fintech startup in Denver with 12 engineers spread across three states. They went with a PPO so each employee could pick a local specialist without jumping through referral hoops. The higher premium was justified because the team values flexibility and the ability to see providers while traveling for conferences.
Finally, a SaaS company in Chicago opted for a POS plan because they liked the HMO‑style cost control but didn’t want to be stuck with zero out‑of‑network options. When a sales rep needed urgent physiotherapy in a neighboring state, the POS covered it at a reduced rate after a quick referral from the PCP.
Quick decision checklist
- How much predictability do you need in monthly premiums?
- Do you have a go‑to clinic or do you need nationwide flexibility?
- Is your team comfortable navigating referrals, or would they prefer “just show up” freedom?
Answering these three questions narrows the field fast.
Actionable steps to pick the right plan
1. Pull the network list from each carrier and map it against where your employees live or travel. If 80 % of your team can see a provider within a 10‑mile radius, an HMO might be fine.
2. Run a cost‑vs‑flexibility scenario. Take the base premium, add an average out‑of‑pocket estimate (deductible + co‑pays), and compare it to the PPO’s higher premium but lower out‑of‑pocket for out‑of‑network visits.
3. Test the referral workflow. Call the carrier’s support line and ask how quickly a PCP can issue a specialist referral. Note the hold time – a long wait can signal a friction point for a fast‑moving team.
4. Check the out‑of‑network policy. Some POS plans only cover emergencies out‑of‑network; others will pre‑authorize certain services. Make sure the policy matches your team’s travel patterns.
5. Document the decision. Create a one‑page cheat sheet that lists the chosen plan’s network rules, referral steps, and cost expectations. Share it on your internal wiki so new hires can get up to speed instantly.
Side‑by‑side comparison
| Feature | HMO | PPO | POS |
|---|---|---|---|
| Network flexibility | Strictly in‑network | In‑network preferred; out‑of‑network allowed | In‑network primary, limited out‑of‑network |
| Referral requirement | Yes, for specialists | No (but may need pre‑approval) | Yes, for specialists |
| Out‑of‑network coverage | Usually none, except emergencies | Partial coverage, higher cost‑share | Partial, higher cost‑share than in‑network |
| Typical cost profile | Lower premiums, higher copays | Higher premiums, lower copays | Mid‑range premiums, mixed copays |
Bottom line: there’s no one‑size‑fits‑all answer. The “right” plan hinges on how your startup balances cost predictability with the freedom to see any doctor you want. Use the checklist, run the quick cost‑vs‑flex test, and you’ll land on a plan that keeps your runway healthy while your team stays covered.
Cost Management Strategies and Tax Benefits
When you stare at that monthly payroll sheet, the health‑insurance line can feel like a silent budget thief. You’ve already picked a plan type – now the real work begins: squeezing value without sacrificing coverage.
First thing’s first – get clear on what you actually control. Premiums are set by the carrier, but the way you design contributions, deductibles, and ancillary benefits is totally in your hands.
Smart cost‑control levers
Ask yourself: could a higher deductible paired with a Health Savings Account (HSA) actually lower the overall spend? The Paychex guide notes that 61% of employers now offer an HSA, letting employees cover out‑of‑pocket costs tax‑free while you keep the premium modest.according to Paychex’s cost‑control overview
Next, involve your team. Run a quick poll on which perks matter most – telehealth, mental‑health apps, or maybe a wellness stipend. Dropping a rarely‑used benefit can shave a few hundred dollars per employee every year.
Another low‑effort win is to encourage employees to use urgent‑care clinics instead of emergency rooms for non‑critical issues. A short education session or a one‑page cheat sheet on “when to call 911 vs. when to book urgent care” can curb claim volume dramatically.
Tax‑saving angles you shouldn’t miss
Group health insurance for startups isn’t just a perk; it’s a tax lever. Premiums you pay on a pre‑tax basis reduce your taxable payroll, and many states offer a small‑business health‑care tax credit that can cover up to half of your costs if you qualify for the SHOP marketplace.
Don’t forget Health Reimbursement Arrangements (HRAs). An HRA lets you reimburse employees for qualified medical expenses tax‑free, and the reimbursement amount is deductible for your business. Take Command explains that HRAs can be a flexible, tax‑advantaged alternative to traditional fully‑insured plans, especially when your headcount is still under 50.Take Command’s HRA overview
Here’s a quick checklist you can copy‑paste into a doc:
- Review eligibility for the SHOP tax credit – plug in your projected payroll and see if you hit the 50% credit threshold.
- Run a cost‑vs‑deductible model: base premium + employer contribution vs. higher deductible + HSA contribution.
- Survey employees on preferred add‑ons (telehealth, mental health, wellness).
- Identify low‑cost utilization‑management tools – telehealth platforms, nurse hotlines, or self‑service portals.
- Set up a quarterly review of claim data to spot trends and negotiate with the carrier.
Remember, the goal isn’t to skimp on care; it’s to align spend with actual usage. If a remote‑first developer never steps foot in a clinic, a telehealth‑heavy plan makes sense. If your sales team travels a lot, a PPO with decent out‑of‑network coverage might be worth the premium bump.
And don’t overlook the power of bundling. Negotiating medical, dental, and vision together often lands you a better rate than buying each line separately. Carriers love the volume, and you love the savings.
Finally, keep the conversation alive. Host a brief “benefits Q&A” every six months, share success stories (like Maya’s team saving 15% on hiring costs), and remind folks that every dollar you save on premiums can be redirected toward product development or a coffee‑fund for the office.
By treating health‑insurance costs as a dynamic, negotiable part of your financial plan – and by leveraging the tax breaks built into the system – you’ll keep your runway healthy while your team stays covered.

Integrating Group Health Insurance with Other Benefits (IUL, Mortgage Protection, Retirement)
Why bundle at all?
When you look at your startup’s balance sheet, health insurance already feels like a line‑item you can’t dodge. But what if that same dollar could also help protect a founder’s mortgage or build a tax‑advantaged cash reserve for later?
That’s the magic of integrating group health insurance with indexed universal life (IUL) policies, mortgage‑protection riders, and retirement accounts. You’re not just buying a doctor’s note; you’re creating a safety net that grows with your company.
Real‑world snapshot: the “three‑piece” strategy
Take Maya’s four‑person app studio again. After she nailed a bronze HRA plan, she added a small IUL for each co‑founder. The policy’s cash‑value component earned a modest, tax‑free return that covered half of her mortgage payment during a slow quarter. At the same time, the startup’s 401(k) match was set at 3 % of payroll, funded through the same payroll deduction system that handled the health premiums.
Result? When Maya’s biggest client delayed payment, the IUL’s cash value paid the mortgage, the 401(k) stayed on track, and the health plan kept the team healthy. The whole package cost her only 2 % more in monthly premiums, but it saved her from a potential cash‑flow crisis.
Step‑by‑step checklist for integration
- Map existing benefits. List every line – health, dental, vision, HRA, retirement – and note the payroll deduction method.
- Identify overlap. IUL policies often include optional mortgage‑protection riders. If you already have a separate mortgage‑protection plan, you might consolidate.
- Calculate tax impact. Premiums for IULs are paid with after‑tax dollars, but the cash value grows tax‑deferred. Use a simple spreadsheet: premium × 12 months = annual cost, then compare the tax‑savings from a higher 401(k) match or HSA contribution.
- Talk to your carrier. Not every group‑health carrier offers IUL add‑ons, but many large insurers do. Ask for a bundled quote that includes a “life‑and‑health” package.
- Communicate the bundle. Draft a one‑page cheat sheet for your team that shows how the health premium, IUL cash value, and retirement match all flow from the same payroll deduction.
- Review quarterly. Track claim data, IUL cash‑value growth, and retirement account balances. Adjust contributions if you see excess cash sitting idle.
Data‑driven benefits of bundling
According to Voya’s employee‑benefits research, companies that combine health insurance with retirement savings options see up to a 12 % boost in employee retention, because workers feel their financial future is being looked after on multiple fronts.Voya employee benefits research
Pan‑American Life notes that adding a mortgage‑protection rider to a life‑insurance policy can reduce the likelihood of “medical bankruptcy” by offering an alternative source of funds during unexpected health events.Pan‑American Life insurance insights
Practical tips to keep the bundle lean
— Start with the smallest IUL face amount that still qualifies for the rider. You can always increase it later when cash flow improves.
— Use a Health Savings Account (HSA) alongside the HRA. The HSA’s tax‑free withdrawals can supplement the IUL cash value if you need a quick bridge.
— Negotiate the mortgage‑protection rider as part of the group‑health contract. Carriers love volume, and they’ll often shave a few hundred dollars off the premium when you bundle three or more products.
Action plan for today
1. Pull your latest payroll report and flag the total health‑insurance deduction.
2. Call your current carrier’s account rep and ask: “Do you offer an indexed universal life policy with a mortgage‑protection rider that can be funded through payroll?”
3. Draft a quick internal memo that outlines the three‑piece benefit, includes the checklist above, and invites employees to a 15‑minute Q&A.
4. Set a calendar reminder for a 90‑day review – look at claim trends, IUL cash‑value growth, and retirement match participation.
If you take these steps, you’ll turn a single health‑insurance line into a multi‑layered financial safety net that protects your team, your founders, and your runway.
Ready to see how it works for your startup? Schedule a free consultation with Life Care Benefit Services and let us design a bundled package that fits your cash‑flow reality.
Implementation Checklist for Startup Founders
Okay, you’ve just decided to bundle group health insurance with the other financial safety nets we talked about. Now it’s time to turn that decision into a concrete plan you can actually follow.
1️⃣ Pull the data you already have
Grab your latest payroll export. You need each employee’s name, age, salary bracket, and the current health‑insurance deduction. If you’ve been using a simple spreadsheet, copy it into a new tab called “Benefits Dashboard.”
Why? Because every later step—whether you’re negotiating a rider or setting a contribution percentage—relies on those numbers.
2️⃣ Talk to your carrier’s rep
Give the account manager a quick call. Ask three things: do they offer an indexed universal life (IUL) with a mortgage‑protection rider, can that be funded through payroll, and what discount do they give for bundling three products?
Take notes in real time. Write down the premium for the base health plan, the extra cost for the IUL rider, and any “startup‑friendly” reduction they mention.
3️⃣ Draft a one‑page benefits memo
Summarize the three‑piece bundle in plain language. Something like: “We’re adding a health plan, an IUL with mortgage protection, and a 401(k) match—all deducted automatically.”
Include the checklist we’re building right now, and invite the team to a 15‑minute Q&A. Keep the memo under a page so people actually read it.
4️⃣ Set contribution percentages
Decide how much of the premium you’ll cover. A common starter is 60 % employer contribution, with employees picking up the rest.
If cash flow is tight, consider a defined‑contribution HRA for the health side and a flat $50 monthly contribution to the IUL. That way the total out‑of‑pocket stay predictable.
5️⃣ Build a simple rollout timeline
Day 1‑3: Pull data and talk to the carrier.
Day 4‑7: Draft memo and get internal sign‑off.
Day 8‑10: Send memo, schedule Q&A, and open enrollment.
Mark a calendar reminder for a 90‑day review. That’s when you’ll compare claim trends, IUL cash‑value growth, and retirement match participation.
6️⃣ Test the enrollment process
Before you hit “go,” run a dry‑run with one volunteer employee. Have them fill out the enrollment form, submit the payroll deduction change, and confirm the carrier receives the data.
If anything breaks—like a missing field or a payment error—fix it now. A smooth first experience builds trust for the whole team.
7️⃣ Track key metrics
Every month, pull three numbers: total health‑insurance cost, IUL cash‑value increase, and the amount matched to 401(k). Plot them on a simple line chart in your Benefits Dashboard.
When you see the cash value climbing or the health claims dropping, you have concrete proof that the bundle is working.
8️⃣ Communicate wins
Every quarter, send a short “Benefits Snapshot” email. Highlight something like, “Our IUL cash value covered $1,200 of Maya’s mortgage last quarter” or “Health‑care claims fell 12 % after we added tele‑health.”
People love numbers that show their paycheck is being put to good use.
So, what’s the next step? Grab that payroll file, set a call with your carrier, and start ticking off the checklist. The more you treat this like a project with clear milestones, the faster you’ll turn a line‑item expense into a multi‑layered safety net for you and your team.
Ready to lock in the bundle? Schedule a free consultation with Life Care Benefit Services today and let us help you fine‑tune every piece.
FAQ
What is “group health insurance for startups” and how does it differ from regular group plans?
Group health insurance for startups is basically the same legal structure—a single contract that covers all your employees—but it’s tailored for smaller, fast‑growing teams. Because you’re often under 50 people, carriers can offer “small‑group” or SHOP products that have lower administrative fees and more flexibility around contribution percentages. In practice that means you can start with a modest premium, add tele‑health or mental‑health apps as optional riders, and scale the plan as you hire. The key difference is the focus on affordability and easy enrollment, not the massive bureaucracy you’d see at a Fortune‑500.
Do I really need to meet the ACA affordability test if I have fewer than 50 employees?
Legally, the ACA’s employer‑shared responsibility kicks in at 50 full‑time equivalents, so a five‑person startup isn’t penalized for not offering “affordable” coverage. Still, offering a plan that meets the 9.5 % of household income benchmark helps you attract talent and avoid future compliance headaches if you grow past the threshold. You can run a quick calculator—multiply an average employee’s salary by 9.5 % and compare that number to the employee’s share of the premium. If it’s lower, you’re already in the safe zone.
How can I keep the monthly cost predictable when my payroll fluctuates?
One trick is to use a defined‑contribution Health Reimbursement Arrangement (HRA) instead of a fully‑insured plan. You set a flat dollar amount each month—say $200 per employee—and let each team member pick the plan that fits their needs. That way the company’s out‑of‑pocket cost stays constant, even if headcount changes. If you prefer a traditional plan, lock in a multi‑year rate with a carrier that offers “rate caps” for the first 12‑18 months; you’ll know exactly what you’ll pay while the business stabilizes.
What should I look for in the provider’s network to avoid surprise out‑of‑pocket bills?
Start by mapping where your core team lives or works. Pull a sample provider list from the carrier’s portal and search for the clinics and hospitals they already trust. If at least three in‑network options exist within a ten‑mile radius of each office, you’re likely safe. Also, verify that specialists—dermatologists, OB‑GYNs, mental‑health counselors—are covered without a referral if your culture values quick access. Ask the rep to walk you through the “out‑of‑network” policy; some plans only cover emergencies, while others will pre‑authorize certain services.
Can I bundle the group health plan with other benefits like IUL or mortgage protection?
Absolutely. Many carriers that handle group health also sell indexed universal life (IUL) policies and mortgage‑protection riders, and they’ll give you a discount when you bundle three or more products. The trick is to run the payroll deduction once and allocate percentages—for example, 60 % of the premium goes to health, 30 % to the IUL rider, and 10 % to the mortgage rider. That way the employee sees a single “benefits” line on their pay stub, and you keep administration simple.
How often should I review the plan to make sure it still fits my startup’s needs?
Treat the benefits package like a quarterly sprint. Every three months pull three numbers: total health‑insurance cost, employee enrollment rate, and any utilization spikes (like a sudden rise in tele‑health visits). Compare those metrics to your original assumptions—are you paying for services no one uses? If the answer is yes, renegotiate the carrier or trim optional add‑ons. Also, schedule a brief “benefits check‑in” with your team; a quick poll can surface hidden preferences before the next open enrollment window.
What’s the first concrete step I should take to get group health insurance for my startup?
Grab a simple spreadsheet and list every employee’s age, salary bracket, and preferred coverage type. Then head to a reputable carrier’s online quote tool and upload that CSV—most platforms will return a price in minutes. Once you have three quotes, compare the premium, employer contribution, and network breadth side by side. Pick the one that balances cost with the doctors your team already trusts, and set up a call with the carrier to lock in the rate. From there you can move on to enrollment and communication.
Conclusion
So you’ve walked through the why, the how, and the nuts‑and‑bolts of group health insurance for startups. If you’re still wondering whether it’s worth the effort, think about the last time a teammate skipped a doctor’s visit because the cost felt like a mystery.
That hesitation costs you more than a few dollars – it costs morale, productivity, and sometimes even talent retention. When you lock in a small‑group plan, you’re not just ticking a compliance box; you’re giving your crew the peace of mind to focus on building the next big thing.
Here’s a quick recap: start with clean data, compare at least three carriers, choose a plan type that matches your team’s workflow, and set a contribution model that keeps the runway healthy. Then, schedule a brief “benefits check‑in” every quarter to tweak what isn’t working.
Does any of this feel overwhelming? It’s okay – the biggest step is simply reaching out for expert help. A short call with Life Care Benefit Services can turn those spreadsheets into a solid, affordable package tailored to your startup.
Ready to protect your people and your bottom line? Schedule a free consultation today and watch your startup thrive with confidence. You’ll see the difference within weeks.