Picture this: you’ve just hired your third employee, and you can already feel the weight of figuring out benefits.
Does the idea of offering health insurance make your stomach flip? You’re not alone—many small‑business owners stare at the same maze of plans and wonder where to start.
What if I told you that setting up coverage doesn’t have to be a nightmare? It can be as straightforward as a coffee chat, especially when you focus on the basics.
First, recognize why you’re even considering this step. A solid health plan helps attract talent, keeps morale high, and protects your team from unexpected medical bills.
Next, take inventory of your workforce. How many full‑time employees do you have? Are any part‑timers eligible for prorated coverage? These answers shape the type of group plan you’ll need.
Then, explore the market. Small businesses often qualify for group policies that are cheaper per person than individual plans. You’ll also discover options that let you customize deductibles and co‑pays to fit your budget.
And here’s a practical tip: start with a needs assessment questionnaire. Ask your staff what they value most—whether it’s low premiums, wide doctor networks, or prescription coverage. Their input will guide you toward a plan that feels like a win‑win.
Once you’ve gathered data, reach out to a trusted broker who can translate the jargon. A good partner will pull quotes, compare carriers, and explain how subsidies might lower your costs.
Speaking of subsidies, many owners don’t realize they may qualify for tax‑advantaged credits that shave hundreds off a monthly premium. That’s a game‑changer if you’re watching cash flow.
Finally, remember that implementation is an ongoing conversation. Set up an easy enrollment portal, schedule a brief benefits meeting, and keep the lines open for questions throughout the year.
Ready to take the first step? Check out our guide on navigating group health insurance for small business owners and start turning uncertainty into confidence.
Take a breath, outline your priorities, and you’ll find that offering health insurance is less a hurdle and more a strategic advantage for your growing team.
TL;DR
Offering health coverage doesn’t have to be a nightmare; follow these steps to learn how to offer health insurance to employees without breaking the bank.
You’ll assess needs, compare plans, secure subsidies, and set up an easy enrollment portal, turning uncertainty into confidence for you and your growing team today.
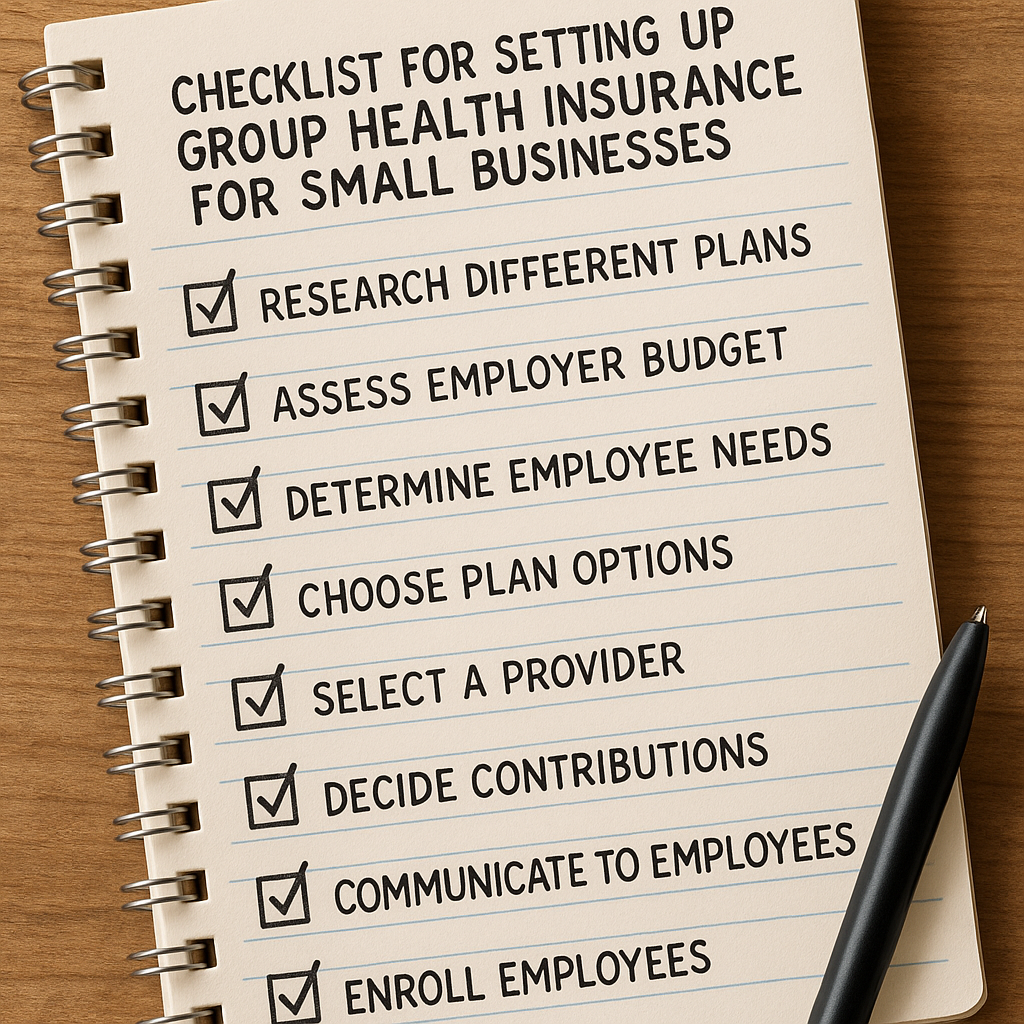
Step 1: Assess Your Business Needs
Before you even think about picking a plan, pause and ask yourself what your business actually needs today. It sounds obvious, but most owners jump straight to pricing and forget the human side. Take a breath, grab a notebook, and imagine you’re sitting down with each team member over coffee.
Map Your workforce composition
Start by listing every employee who works 30 hours or more per week – that’s the group that the Affordable Care Act counts as full‑time. Note any part‑timers who might qualify for prorated coverage; some carriers let you extend benefits to them for a modest extra cost.
For example, a boutique design studio with four full‑time designers and two part‑time interns might choose a core plan for the full‑timers and a supplemental “pay‑as‑you‑go” option for the interns. That way you’re not overpaying, but you still show you care.
Identify what matters most to your people
Run a quick, informal survey. Ask questions like “Do you prefer lower monthly premiums or lower out‑of‑pocket costs?” or “Is a wide doctor network a deal‑breaker for you?” Real answers will steer you toward plans that feel like a win‑win.
One small‑business owner I know asked his crew: “If you could pick one benefit besides health, what would it be?” The most common answer was dental coverage, which led him to bundle dental with the health plan – a move that saved about 12% on overall costs because the carrier offered a discount for bundled services.
Calculate your budget ceiling
Pull your latest payroll report and decide what percentage of payroll you’re comfortable allocating to benefits. Many businesses aim for 5‑7% of total compensation. If your payroll is $250,000 a year, that gives you $12,500‑$17,500 for health‑related expenses.
Remember that premiums are tax‑deductible, and you might qualify for the Small Business Health Care Tax Credit, which can cover up to half of your contribution. A quick chat with your accountant can turn a vague budget line into a concrete, tax‑advantaged number.
Sketch a rough cost model
Take the average premium for a small‑group plan (often around $450 per employee per month) and multiply by the number of full‑time staff. Then apply your planned employer contribution – say 70% – to see the out‑of‑pocket amount you’ll actually pay.
Example: 5 full‑time employees × $450 × 70% = $1,575 per month, or $18,900 per year. Add any optional add‑ons (vision, life) and you have a realistic ballpark.
Consider future growth
Ask yourself where you see the company in 12‑18 months. If you plan to hire three more people, choose a plan that scales without a massive jump in per‑person cost. Some carriers offer “tiered” pricing that rewards you as claims stay low, which can be a smart hedge against rapid hiring.
And don’t forget about seasonality. A retail shop that swells during holidays might need a flexible enrollment window, while a tech startup with steady headcount can lock in a multi‑year rate.
Summarize your findings
Create a one‑page cheat sheet that captures:
- Total full‑time headcount
- Key benefits employees care about (e.g., low copays, dental)
- Budget ceiling and employer contribution target
- Potential tax credits or subsidies
- Scalability needs
When you walk into a broker’s office with this sheet, you’ll cut the fluff and get straight to the options that actually fit.
So, what’s the next move? Take the cheat sheet, share it with your team for a quick “does this look right?” check, then schedule a call with a licensed agent who can pull real quotes based on these parameters.
That’s the foundation – a clear picture of who you are, what they need, and how much you can spend. With that in hand, the rest of the process becomes a lot less intimidating.
Step 2: Choose the Right Plan Types
Now that you’ve got a clear picture of headcount, budget, and what your team really wants, the fun part begins—picking the plan type that actually works for you.
Know the three basic families of group coverage
Most small employers fall into one of three buckets: fully‑insured, self‑funded, or level‑funded.
A fully‑insured plan is the classic “pay‑the‑carrier” model; the insurer assumes the risk and you pay a fixed premium each month. That’s the easiest route if you like predictable bills.
Self‑funded (or “self‑insured”) means you pay claims out‑of‑pocket and the carrier only provides administrative services. It can save money when claims are low, but you need a cushion to cover spikes.
Level‑funded is a hybrid: you fund an estimated claim amount each month, and the carrier refunds any excess at year‑end. It gives you some risk protection without the full premium of a fully‑insured plan.
Factor in tax‑advantaged options
Many groups pair a primary health plan with a Health Savings Account (HSA) or a Health Reimbursement Arrangement (HRA). An HSA lets employees stash pre‑tax dollars for deductibles, copays, and qualified expenses—often lowering overall costs. An HRA is employer‑funded, reimburses qualified expenses tax‑free, and any unused balance can roll over.
Both tools are described on HealthCare.gov’s small‑business coverage guide, which explains how they can reduce your taxable payroll and give staff more flexibility.
Match plan features to what your people care about
Remember the survey you ran in Step 1? Pull those answers into a quick decision matrix. If most of your crew said “low premiums,” look for high‑deductible plans paired with HSAs. If they shouted “wide doctor network,” prioritize PPOs or plans with national provider directories.
- Network size – PPO vs. HMO vs. EPO
- Deductible level – high vs. low
- Out‑of‑pocket max – keep it below the ACA limit if possible
- Prescription coverage – tiered formulary can save big bucks
- Additional perks – telehealth, wellness apps, dental bundles
Sketch a simple spreadsheet: column A = plan name, B = monthly premium, C = employer contribution %, D = deductible, E = employee out‑of‑pocket max. Highlight the rows that meet your budget ceiling and employee preferences.
Don’t overlook special programs
If you’re in the federal sector or have employees who are eligible for the Federal Employee Health Benefits (FEHB) system, the OPM comparison tool can help you see plan benefits side‑by‑side. Check the OPM plan comparison page for official benefit summaries before you commit.
Even if you’re not a federal employee, the layout of that tool is a handy template for any broker’s side‑by‑side quote sheet.
Watch a quick walkthrough
Sometimes seeing the process in action clicks better than any checklist. Below is a short video that walks you through comparing plan types, spotting hidden fees, and aligning choices with your cheat sheet.
Action checklist for today
Grab a pen and run through these four items before you call a broker:
- Identify which family (fully‑insured, self‑funded, level‑funded) fits your cash‑flow comfort.
- Decide if you’ll add an HSA or HRA based on employee survey results.
- Fill in the spreadsheet matrix with at least three plan options that meet your budget.
- Bookmark the OPM and HealthCare.gov pages for quick reference when quotes arrive.
When you walk into that meeting armed with this list, you’ll steer the conversation toward the plans that actually solve your problem—not the ones that just sound fancy.
Step 3: Compare Providers & Costs
Now that you’ve narrowed down the plan families, it’s time to put the numbers side by side and see which carrier actually fits your budget and your team’s needs. This is where the “compare providers & costs” part of how to offer health insurance to employees becomes less intimidating and more like a coffee‑shop spreadsheet session.
Gather your quote packets
Ask each broker for a clean quote sheet that lists the premium, employer contribution percentage, deductible, out‑of‑pocket max, and any ancillary fees. If a carrier throws in a “setup fee” or “administrative surcharge,” write it down – those little line items can balloon the total cost.
Tip: request the same coverage level from every provider (e.g., 70% employer contribution, PPO network) so you’re comparing apples to apples.
Create a comparison grid
Take a blank spreadsheet and drop the columns you care about. Here’s a quick starter layout:
- Provider name
- Monthly premium (total)
- Employer % contribution
- Deductible
- Network size (local, regional, national)
- Hidden fees (setup, termination, claim‑processing)
Plug the numbers in and watch the differences pop out. You’ll often see one carrier with a lower premium but a higher deductible, while another might charge more up front but give a richer network.
Spot hidden fees
Ever looked at a premium and thought, “That’s a steal,” only to discover a $150 per‑member‑per‑month (PMPM) admin fee? Those costs aren’t always highlighted in the headline quote. Ask directly:
- Is there a charge for adding or dropping an employee mid‑year?
- Do you pay per claim processed, or is it baked into the premium?
- What happens to unused HSA contributions – any rollover penalty?
Getting clear answers now saves surprise invoices later.
Evaluate total cost of ownership
Take the premium, subtract the employer contribution, then add any recurring fees. Finally, estimate the average out‑of‑pocket spend your team will face based on the deductible and co‑pay structure. A simple formula looks like this:
Total monthly cost = (Premium × (1 – Employer %)) + Hidden fees + Estimated employee share
If the numbers still feel fuzzy, run a quick “what‑if” scenario: what if half your staff hit the deductible? That helps you decide whether a high‑deductible HSA‑compatible plan truly saves money.
Make a decision
Now compare the rows in your grid. Highlight the plan that meets three criteria: stays under your budget ceiling, aligns with the benefits your survey revealed, and has the fewest surprise fees. If two options are neck‑and‑neck, let the network size or customer service reputation be the tie‑breaker.
When you’ve picked a winner, reach out to the broker, confirm the final quote, and ask for a sample enrollment portal. Seeing the user experience before you sign the contract can reveal hidden usability costs that affect employee satisfaction.

| Provider | Monthly Premium | Employer % | Deductible | Network | Notable Fees |
|---|---|---|---|---|---|
| Carrier A | $420 | 70% | $1,200 | National PPO | $0 admin fee |
| Carrier B | $380 | 65% | $2,500 | Regional HMO | $150 PMPM admin |
| Carrier C | $440 | 75% | $1,000 | Local PPO | $0 setup, $50 termination |
Before you lock anything in, double‑check the renewal terms. Some carriers automatically raise premiums by a set percentage each year, while others tie increases to claim experience. Knowing the escalation rule lets you forecast next‑year costs and keep your budget on track.
And remember, the cheapest option isn’t always the best fit for your culture.
Take a deep breath, trust the numbers you just crunched, and schedule a quick call with your chosen broker. That conversation is the final piece that turns your comparison into a concrete benefits package you can roll out to your team.
Step 4: Communicate the Benefits to Employees
Start with a simple story
Imagine you just rolled out a new health plan and, two weeks later, you hear Sarah from accounting say, “I finally get why we’re paying that premium.” That moment of “aha” is the sweet spot we’re aiming for.
When you’re figuring out how to offer health insurance to employees, the real work begins after the paperwork is signed – you have to make the benefits feel tangible.
Pick the right mix of channels
People skim email, binge a quick video, or flip through a printed handbook. Don’t bet on just one method.
Start with a short, in‑person (or Zoom) huddle. A 15‑minute session lets you read the room, answer live questions, and bust jargon on the spot. Follow up with a one‑page cheat sheet that breaks down premium costs, what the employer covers, and any employee‑paid portions.
Upload the same cheat sheet to your internal portal so anyone can pull it up later. A quick FAQ page that lives on the same site keeps the information evergreen.
Speak their language
Instead of saying “deductible,” say “the amount you pay out of pocket before the plan kicks in.” Swap “out‑of‑pocket maximum” for “the most you’ll ever pay in a year, no matter what you need.” Those tiny swaps cut confusion in half.
Use real examples: “If you need a surgery that costs $5,000, you’ll pay the $1,200 deductible, then the plan covers the rest.” Concrete numbers stick better than abstract promises.
Leverage digital tools
Send a short video walkthrough that shows the enrollment portal, highlights where to find the cost breakdown, and demonstrates how to submit a claim. Keep it under three minutes – people lose patience after that.
Pair the video with an email that includes a quick poll: “Which part of the plan still feels fuzzy?” The responses tell you where to focus your next live Q&A.
Address common roadblocks head‑on
Many employees feel overwhelmed by the sheer number of options. Acknowledge that: “I get it – health insurance can feel like a maze.” Then give them a decision tree: premium‑focused, network‑focused, or out‑of‑pocket‑focused.
According to clear communication improves employee engagement and satisfaction, simplifying the language and offering multiple touchpoints makes staff more confident in their choices.
Make it a two‑way conversation
Open a dedicated Slack channel or a mailbox where people can drop questions any time of day. Rotate a “benefits buddy” each week – a peer who’s already enrolled and can share personal tips.
Gather feedback after the open enrollment period. A one‑line survey like “Did you feel you had enough info to pick the right plan?” gives you a quick health check and shows you care about continuous improvement.
Legal notices, but not a snooze‑fest
Yes, you need to provide required notices – summary plan descriptions, ERISA statements, and any state disclosures. Slip those into the same PDF you’re already sending; label the section clearly so it doesn’t get lost in the fluff.
Make the legal part a distinct appendix, then reference it in plain language: “The next few pages cover the legal stuff you’re required to see – you can skim them now or later, but they’re there for completeness.”
Wrap up with a clear call to action
End every communication with a single, unmistakable next step: “Log into the portal by Friday, March 15, and select your coverage.” Add a deadline, a brief reminder of the deadline’s purpose, and a friendly nudge that you’re there to help.
Finally, celebrate the rollout. Send a quick “thanks for joining” note, maybe with a small perk like a coffee gift card, to reinforce that you value their participation.
When you blend face‑to‑face moments, bite‑size digital resources, and an open feedback loop, you turn a complex benefit into a confident, appreciated part of your workplace culture.
Step 5: Implement and Manage the Plan
Alright, you’ve picked the plan, you’ve got the numbers in a spreadsheet, and the team is buzzing with excitement. Now comes the part that feels a lot like launching a small rocket: you actually put the benefit into motion and keep it humming.
Set up the enrollment portal – the digital front door
First thing’s first: get an easy‑to‑use enrollment platform live at least 30 days before the official start date. Most carriers will give you a branded portal, but you can also use a third‑party tool that syncs with your payroll system. The goal is one click to log in, one click to select a plan, and a clear “Done!” confirmation.
Pro tip: add a short, 60‑second walkthrough video right on the login page. A quick visual cue cuts confusion in half, and employees love seeing a friendly face (even if it’s a recorded one).
Collect a clean employee census
Before you hit “Submit” on the carrier’s paperwork, double‑check your census. That means name, date of birth, SSN, and % of full‑time hours. A tiny typo can cause a claim to be denied later, and nobody wants that headache.
Here’s a real‑world example: a boutique marketing firm in Denver discovered two of its designers were mistakenly listed as part‑time. Because the plan required a 30‑hour minimum, those employees missed the first month’s coverage. The fix? A simple Excel validation rule that flags anyone under 30 hours before the final upload.
Communicate the go‑live date and next steps
Remember the “story” you told in Step 4? Now you deliver the next chapter. Send a brief email (or Slack note) that says, “Your benefits portal opens on Monday, March 18. Log in by Friday, March 22 to lock in your choice.” Include the deadline, a link to the portal, and a line that says you’re available for live Q&A.
And don’t forget a gentle reminder a day before the deadline – a friendly nudge works better than a stern “deadline missed.”
Run a live enrollment session
Schedule a 30‑minute Zoom (or in‑person) walk‑through. Start by sharing your screen, click through the portal, and answer the top three questions you’ve seen in the FAQ: “What does ‘deductible’ really mean?” “Can I add my spouse later?” “How do I claim my HSA?”
During the session, ask participants to type any confusing wording they see. Capture those pain points and update the portal FAQ on the fly. This real‑time feedback loop makes the rollout feel collaborative, not top‑down.
Track enrollment metrics daily
Set up a simple dashboard that shows:
- Total employees invited
If you’re using a payroll‑integrated system, you can pull the data automatically; otherwise, a shared Google Sheet works fine for a small team. Aim for at least 80% enrollment within the first two weeks – anything lower is a signal to fire off a reminder.
Handle changes and mid‑year updates
Life happens: an employee gets married, a new hire joins, or someone goes on a six‑month leave. Your plan should have a clear “change window” (often 30 days after a qualifying life event). Document the steps:
- Employee notifies HR via a short form.
- HR updates the census in the carrier’s portal.
- Employee receives a confirmation email with new coverage details.
Keeping this process tight prevents costly re‑enrollment errors and keeps the carrier happy.
Stay on top of compliance and reporting
Under the ACA, if you offer coverage to full‑time staff you must offer it to all similarly situated workers. The HealthCare.gov guide notes that a plan is “affordable” when employee premiums are under roughly 10% of household income. Run a quick audit each year to confirm you stay under that threshold, especially if you raise premiums.
Also, keep a copy of the Summary Plan Description, ERISA notices, and any state disclosures in a shared folder. When an employee asks, you can point them to “the legal appendix” without digging through piles of paper.
Gather feedback and iterate
After the first enrollment cycle, send a short pulse survey: “What part of the enrollment process was smooth? What could be better?” Use a 5‑point scale and one open‑ended comment box. Analyze the results and prioritize one improvement for the next year – maybe a mobile‑friendly login or clearer language around co‑pays.
One small bakery in Portland used the survey to learn that employees wanted a “quick view” of total out‑of‑pocket costs. They added a simple calculator widget to the portal, and enrollment jumped from 68% to 92% the following year.
Keep the conversation alive
Benefits aren’t a set‑and‑forget item. Schedule a brief “Benefits Check‑In” at your quarterly all‑hands meeting. Share any changes in plan costs, highlight wellness resources, and remind folks about the HSA contribution deadline.
By treating the plan like a living program – with clear steps, regular check‑ins, and a willingness to tweak – you turn “how to offer health insurance to employees” from a one‑off project into an ongoing perk that truly supports your team.
Conclusion
So you’ve walked through the whole process – from figuring out who needs coverage to picking a plan, setting up the portal, and keeping the conversation alive.
When you think about how to offer health insurance to employees, the secret isn’t a magic formula; it’s a series of small, intentional steps that make the whole thing feel like a natural part of your workplace culture.
Remember to start with a clear snapshot of your team’s size and budget, then match those numbers to a plan family that fits your cash‑flow comfort.
A quick survey can surface the features your crew actually cares about, and a simple comparison grid keeps hidden fees from sneaking in.
Implementation is where the rubber meets the road: a clean enrollment portal, a live walkthrough, and daily enrollment metrics keep momentum high.
And don’t forget the feedback loop – a short pulse survey after the first open enrollment can point you to the next tweak that boosts participation.
Does any of this feel overwhelming? That’s okay.
Take one step at a time, lean on a trusted broker, and treat the benefits program like a living conversation.
Ready to turn the plan into a real perk for your team? Reach out today and let us help you design a hassle‑free health benefits experience.
FAQ
What’s the first thing I should do when I decide to offer health insurance to employees?
Start with a quick snapshot of who’s eligible – count full‑time staff, note any part‑timers who might qualify, and pull together a simple budget range. A one‑page cheat sheet that lists headcount, the maximum premium you can afford, and any tax credits you might tap into becomes the compass for every next step. It feels less like a project and more like a conversation you’re having with yourself and your team.
How can I choose the right type of group plan for a small business?
Think about three families: fully‑insured, self‑funded, and level‑funded. If you prefer predictable monthly bills, the fully‑insured route is usually safest. If you have a stable claim history and a cash cushion, self‑funded can shave dollars off the premium. Level‑funded sits in the middle – you fund an estimate and get refunds if claims run low. Match the family to your cash‑flow comfort and the risk you’re willing to take.
Do I really need a broker, or can I go it alone?
Most small owners try to DIY and end up tangled in carrier jargon. A broker acts like a translator who pulls side‑by‑side quotes, flags hidden fees, and points out subsidies you might qualify for. It’s not a cost you can’t afford – the time you save and the potential premium reductions usually pay for themselves within the first year. Think of the broker as a guide who keeps the process from feeling like a maze.
What are the hidden fees I should watch out for in health‑insurance quotes?
Besides the headline premium, carriers love to sprinkle in admin fees, set‑up charges, and per‑member‑per‑month (PMPM) processing fees. Ask directly: “Is there a cost for adding a new hire mid‑year?” or “Do you charge per claim?” Write every extra line item in a comparison grid; the plan with the lowest total cost of ownership often wins, even if its headline premium looks a bit higher.
How do I keep employees engaged during open enrollment?
People absorb info in bursts. Kick off with a live 15‑minute huddle where you walk through the portal, then follow up with a one‑page cheat sheet and a short video walkthrough under three minutes. Open a Slack channel or a dedicated inbox for questions, and sprinkle quick polls after each touchpoint to see what’s still fuzzy. When you treat enrollment as a two‑way conversation, participation jumps from “maybe” to “I’m in.”
What should I do if an employee wants to change their coverage mid‑year?
Most plans allow a 30‑day change window after a qualifying life event – marriage, birth, or a new hire. Create a tiny form where the employee submits the event, you update the carrier’s census, and then you send a confirmation email with the new effective date. Keeping that loop tight avoids missed coverage and prevents costly re‑enrollment errors.
How can I make sure my health‑insurance offering stays affordable over time?
Run an annual audit against the ACA’s affordability threshold (roughly 10 % of household income) and compare your current premium to the budget you set at the start. If premiums creep up, revisit the plan family – maybe a high‑deductible option with an HSA now makes more sense. Also, track renewal clauses: some carriers tie increases to claim experience, others to a flat percentage. Knowing the rule lets you forecast next year’s cost and negotiate smarter.