Let’s be honest: figuring out how to choose Medicare Part D prescription plan feels like standing in a candy store with no clue what to grab. It’s overwhelming, right? You want coverage that fits your medications, budget, and lifestyle—but where do you even start?
Your hope is to find a plan that won’t make you drown in paperwork or surprise you with unexpected costs. And honestly, the stakes feel high, because this isn’t just about saving money—it’s about your health and peace of mind.
Here’s what I’ve learned: there’s no one-size-fits-all solution. What works for your neighbor might not work for you. That’s why knowing exactly how to choose Medicare Part D prescription plan means digging a little deeper into the details that matter most to you personally.
Think about it this way—some plans cover your medications fully, others just partially, and a few won’t cover some drugs at all. Plus, premiums, deductibles, and copays can vary widely. You want to avoid the common trap of picking a plan based on just the monthly cost and later realizing it’s more expensive when you need those prescriptions filled.
So, what’s the secret? It’s all about balance. Understanding what you need vs. what the plan offers. And don’t worry—we’re going to walk through this together, step by step, so you’re not left guessing.
Before diving into the nitty-gritty, keep in mind this isn’t about rushing. Taking your time now means fewer headaches later. And when you’re ready, experts like those at Life Care Benefit Services can help you sort through options tailored just for your unique health situation and finances.
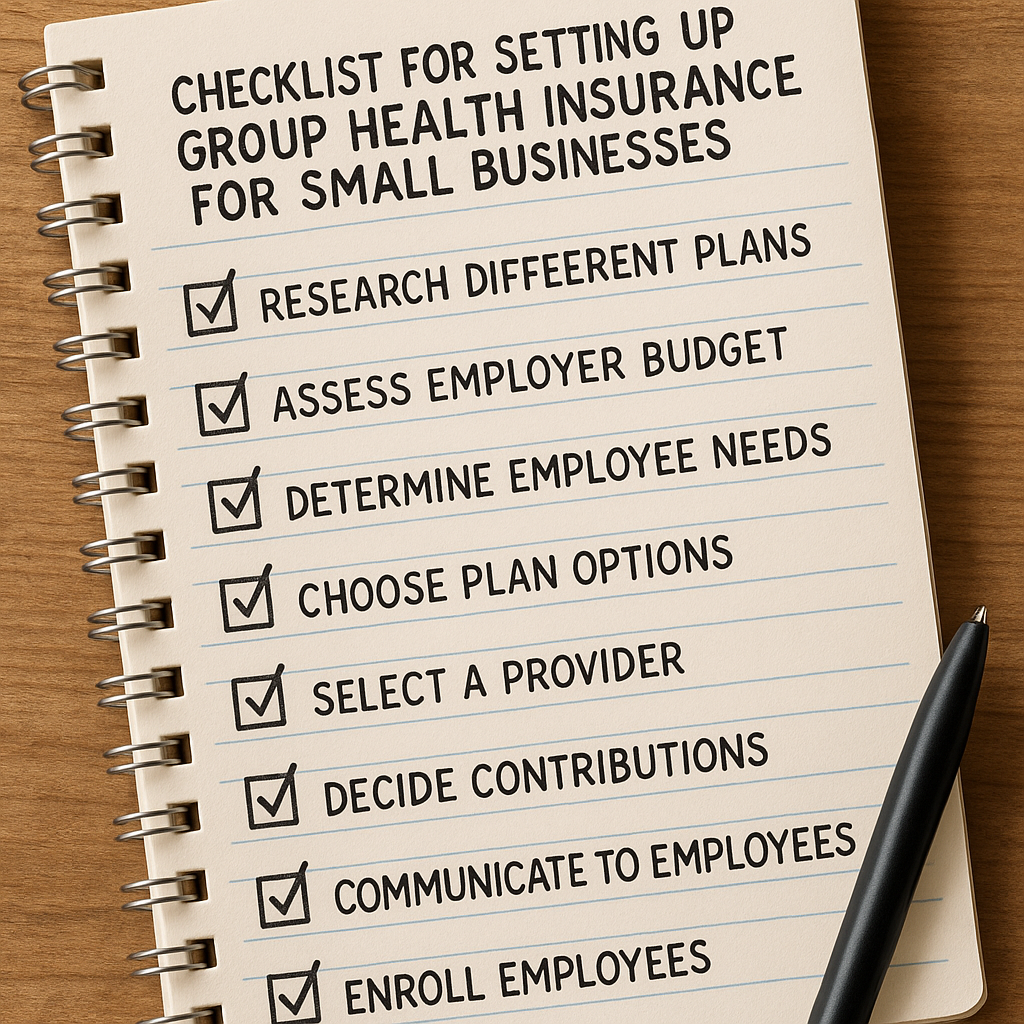
By the end, you’ll know exactly how to choose Medicare Part D prescription plan with confidence—and maybe even a little relief. If you’re curious about navigating insurance for small business owners or family health plans, check out this helpful guide on navigating group health insurance for small business owners. Trust me, making informed choices feels way better than winging it.
Ready? Let’s dive in.
TL;DR
Choosing the right Medicare Part D plan isn’t about just picking the cheapest monthly premium. It’s about balancing costs with coverage—making sure your prescriptions are covered when you need them without surprises.
Take your time, compare plans based on your meds, and don’t hesitate to get personalized help to avoid costly mistakes down the road.
Step 1: Understand Your Prescription Needs and Coverage Requirements
Let’s face it: figuring out how to choose Medicare Part D prescription plan can feel overwhelming. You’re probably staring at a mess of drug names, confusing coverage rules, and premiums that don’t line up with what you actually need. But before you get buried in the fine print, take a breath. The best place to start is right where it counts—your specific prescription needs and how coverage works.
Think about your daily routine. What prescription drugs are you actually taking right now? Write them down. Include dosages, how often you take them, and even the pharmacy you prefer. This isn’t just busywork. Your future Medicare Part D plan hinges on this list. If a plan doesn’t cover your meds or forces you into complicated hoops, it won’t save you money, no matter how low the premium looks.
Here’s where most people trip up: not all Medicare Part D plans cover every drug. Each plan has a list called a “formulary,” which says exactly which medications are included—and sometimes not. You’ll want to find a plan whose formulary matches your prescription list as closely as possible.
Why coverage rules actually matter
Coverage isn’t just about whether your drug is on the formulary. Plans may have rules like prior authorization, step therapy, or quantity limits. For example, have you ever heard of step therapy? It’s like a gatekeeper that requires you to try a cheaper drug before the plan agrees to pay for the one your doctor originally prescribed. Sounds tricky, right? But knowing this upfront can save you stress and surprise costs down the road.
Or maybe your drug requires prior authorization—a kind of permission slip from your insurance plan, saying the drug is medically necessary before they cover it. These kinds of rules vary wildly from plan to plan, so you’ll want to dig into the details. Your prescriber can help by providing supporting info if exceptions are needed.
Coverage gaps and penalties to watch for
Even if you’re not currently taking any medications, it’s worth considering Medicare Part D. Missing the initial enrollment window can trigger a late enrollment penalty—basically, a surcharge on your monthly premium for every month you delayed signing up without creditable drug coverage. This penalty stacks up fast and stays with you for as long as you have Medicare drug coverage.
The good news? You can avoid this by enrolling on time or proving you had other credible drug coverage beforehand. For more on how this works and coverage details, the official Medicare.gov Part D overview explains it clearly.
How to make this all manageable
Start by gathering your prescription info, then check multiple Part D plans’ formularies and coverage rules. Look closely for any prior authorizations or step therapies that could affect your current medications. This isn’t just crossing off a checklist—it’s about making sure your meds are actually covered without hoops that cost extra time and money.
If you want a helping hand, reach out to someone who knows the ropes. Experts like the folks at Life Care Benefit Services can walk you through your options based on your unique needs. No guesswork, just clear guidance.
So, what should you do next? Gather your current prescription list, peek at formularies that match, and don’t ignore those pesky rules around coverage. Remember, the goal here is a plan that fits your life—not the other way around.
Step 2: Compare Different Medicare Part D Plans and Their Formularies
Alright, so you’ve got your prescription list in hand. Now what? Here’s where things can get a bit tricky, but stick with me—it’s absolutely doable and worth the effort.
Think about it this way: not all Medicare Part D plans are created equal. It’s like shopping for groceries—just because two stores have the same milk brand, doesn’t mean their prices or the quality of their selection match. Same deal with Part D plans and their formularies, which are just fancy terms for the list of drugs each plan covers.
So, why compare formularies closely? Because a plan might cover your medication but slap on some annoying rules. For example, your drug might require a prior authorization—meaning your doctor has to get approval before the plan pays. Or there could be step therapy, where you first have to try more affordable drugs before the plan will cover the one your doctor originally prescribed. These rules can cause frustrating delays and sometimes extra costs.
How to start comparing Medicare Part D formularies
Begin by checking if your exact prescriptions are covered. Look up each plan’s formulary—most insurers let you do this online. Pay attention not just to coverage but to the “tier” your drugs fall into since that affects your copays or coinsurance.
Here’s a quick checklist to make your comparison easier:
- Is every medication you currently take included?
- What are the out-of-pocket costs for each drug?
- Are there any step therapy or prior authorization requirements?
- Does the plan prefer generic versions or specific brands?
- Are there quantity limits that might slow you down?
Answering these questions will save you from unexpected surprises later.
One good tip that not everyone mentions: figure out where your pharmacy fits into the plan’s network. Some plans work only with specific pharmacies or offer better prices at their preferred ones. So, if the plan’s formulary looks great but you have to switch to a pharmacy across town, that might not be worth it.
Are you already feeling overwhelmed? Yeah, it’s a lot. But a little diligence here can mean better coverage and less hassle with those stubborn pharmacy calls.
And speaking of tools, don’t forget about the official Medicare Plan Finder. It’s free and lets you plug in your meds, preferred pharmacies, and location to compare plans side by side. Seriously, it’s like having a map when you’re lost in a new city.
Also, keep in mind the 2026 limit on out-of-pocket costs: once you hit $2,100 for covered drugs, you don’t pay more for your meds through the year. This cap only applies to drugs inside the plan coverage, so cross-reference your formulary carefully to see what counts. More details are available on Medicare.gov.
Why you can’t just pick the cheapest plan
It’s tempting to go for the lowest premiums, right? But here’s what most folks don’t realize: a cheap plan with poor formulary coverage might end up costing you way more if your meds aren’t well covered.
Imagine this: You choose a low-cost plan, then find out your crucial blood pressure medication isn’t covered or needs some expensive prior approval. Suddenly, you’re juggling doctor visits, paperwork, and extra out-of-pocket payments. Ain’t nobody got time for that.
So, the secret sauce is balance. Compare plans not only by premiums but by how your specific meds fit into their formulary, the rules that come with that, and pharmacy access.
If you want to skip the headaches, experts at Life Care Benefit Services can help you navigate this maze. They’ve got access to over 50 top-rated insurance carriers and can zero in on plans tailored for you. It’s like having a trusted friend in this confusing system.
Ready to dig in? Start by lining up your drug list, open the Medicare Plan Finder, and check multiple formularies. Don’t rush. Take your time—it’s worth it to find a Part D plan that works like a glove.
Step 3: Evaluate Plan Costs: Premiums, Deductibles, Copayments, and Coverage Gap
Alright, we’ve talked about why the cheapest plan isn’t always the best, but now it’s time to roll up your sleeves and get into the nitty-gritty: what you’ll actually pay for your Medicare Part D plan. Because let’s be honest, the costs here can be a bit like a choose-your-own-adventure game — and picking the wrong path can sting your wallet more than you expect.
So, how do you break down these confusing terms — premiums, deductibles, copayments, and that annoying coverage gap — into something that actually makes sense? Let’s tackle each one, so you can figure out which plan won’t just look good on paper, but also in your bank account.
Premiums: Your Monthly Price Tag
Think of your premium as the monthly subscription fee you pay just to have the plan. It’s that fixed amount you’ll pay whether you use your prescription benefits or not. Some plans lure you in with a low premium, which feels like a bargain, right? But remember, paying less upfront might mean higher costs down the road.
And keep in mind, if you wait too long to sign up for Part D without having other creditable drug coverage, you might face a late enrollment penalty. This penalty stacks on your premium and sticks around as long as you keep drug coverage. Ouch.
Deductibles: Your Out-of-Pocket Kickoff
Deductibles are like the gatekeeper to your insurance. Before your plan starts chipping in on your prescriptions, you’ll need to spend a certain amount out of pocket first. Some plans waive the deductible, which is a nice perk, but others might have it set anywhere from $0 up to a few hundred dollars.
Does a high deductible scare you? Totally understandable. But here’s the kicker: plans with low premiums often have high deductibles, so you might end up paying more upfront when you fill your meds. It’s about balancing what you can afford monthly against what hits your wallet when you actually need the drugs.
Copayments and Coinsurance: Sharing the Cost
Once you’re past the deductible, copayments or coinsurance come into play. These are your share of the cost for each medication, which can be a flat fee — like $10 per prescription — or a percentage of the drug’s price.
Here’s what trips people up: the copayment for a generic drug might be low, but if your medication is brand-name or specialty, that copay or coinsurance can be significantly higher. That’s why checking how your specific meds are treated in a plan is crucial.
What About the Coverage Gap? (Spoiler: It’s Changed)
You might remember hearing about the infamous “donut hole”—a period when drug costs used to spike unexpectedly. Good news: starting in 2025, the coverage gap essentially disappeared, replaced by a smoother cost-sharing system during your drug coverage stages.
Now, instead of sudden price jumps, you move through three phases: deductible, initial coverage, and catastrophic coverage — the latter kicking in when your out-of-pocket costs get really high, and your expenses drop dramatically. It’s a relief for many, but you’ll still want to watch your total costs closely.
Putting It All Together: What to Watch For
Choosing a plan after sizing up these costs can feel like juggling flaming torches. Here’s a quick checklist to help:
- Look beyond the premium: What’s the deductible? How much will you pay for your medications in copays or coinsurance?
- Check if your meds are covered before the deductible or only after — that matters.
- Consider how many prescriptions you take and their cost tiers.
- Don’t forget the late enrollment penalty if you’ve delayed signing up.
- Keep an eye on your expected annual drug expenses, not just monthly fees.
If you’re scratching your head, that’s normal. Life Care Benefit Services can help you compare these tricky cost factors across plans from over 50 carriers, so you don’t have to go it alone.
Still wondering if a plan’s overall cost fits your budget? Sometimes it’s helpful to actually map out your yearly spending, factoring in all the premiums, deductibles, and copays based on your current prescriptions. This gives you a better snapshot of what you’ll really shell out versus what looks cheaper upfront.
| Cost Element | What It Means | Why It Matters |
|---|---|---|
| Premium | Monthly fee to have the plan | Low premium can mean higher other costs; adds up monthly |
| Deductible | Amount you pay before coverage starts | High deductible means more upfront spending before plan pays |
| Copayments/Coinsurance | Your share per prescription | Varies by drug type; impacts out-of-pocket costs for meds |
| Coverage Gap | Phase after initial coverage where costs changed (donut hole) | Now mostly eliminated, but watch for total out-of-pocket limits |
So, what should you do next? Start jotting down your monthly prescriptions, estimate how much you pay now, and then compare that to what each plan’s cost structure would mean year-round. This step isn’t fun, but it’s the best way to avoid surprises and pick a Medicare Part D plan that truly works for you.
Need a hand figuring out these numbers? Medicare’s official guide breaks down costs clearly, and experts at Life Care Benefit Services are just a call away to make sense of it all and get you set up with a plan that fits your meds and your budget.
Step 4: Consider Pharmacy Network Options and Convenient Access
Picking a Medicare Part D plan isn’t just about premiums and copays — where you actually get your prescriptions filled can make a big difference in cost and convenience. Have you ever stood in line at the pharmacy, thinking, “Is this the cheapest place to get my meds?” Yeah, me too. That’s why this part matters more than you might think.
Most Medicare Part D plans have a network of pharmacies they work with, called “in-network pharmacies.” These pharmacies agree to offer discounts to plan members, which usually means lower out-of-pocket costs for you.
Imagine this: You have a plan that prefers a certain pharmacy nearby. If you fill your prescriptions there, you might pay a reduced copay or coinsurance compared to using a pharmacy outside the network. On the other hand, if you go to a pharmacy that’s not in the network, you could end up paying a lot more — even for the same medications.
Do you have a favorite pharmacy? That’s a good starting point. Check if it’s in the network for the plans you’re considering. If it isn’t, you might want to weigh how much hassle and extra cost that could bring.
Why preferred pharmacies matter
Preferred pharmacies are like your plan’s VIPs. They’ve agreed to charge less, and your plan encourages using them. Some plans even use “preferred pharmacy networks” to steer members towards these cost-saving options.
Studies show that people who switch to these preferred pharmacies can save over a hundred dollars a year on average. That’s not pocket change, especially if you’re juggling multiple prescriptions.
But here’s the thing — it’s not just about savings. Location and convenience count big time. If your preferred pharmacy is miles away or difficult to get to, those savings might not feel worth it.
What about getting meds delivered?
Lots of Medicare Part D plans offer mail-order services. You can get up to a 90-day supply of your meds sent right to your doorstep. Think about coming home and finding your prescriptions waiting for you — no lines, no driving, just convenience.
Some plans even have automatic refill programs that reorder your meds before you run out. If you take maintenance medications (like blood pressure or diabetes meds), this can save you time and hassle.
But before you jump on mail order, check if your plan offers it and whether there are any cost benefits like lower copays. Not every plan’s mail-order option is created equal.
So, what should you do next?
Start by looking up the pharmacy network for each plan you’re considering. Ask yourself these questions: Is my pharmacy in the network? Does the plan have nearby preferred pharmacies? Do mail-order options fit my lifestyle?
It’s worth calling your current pharmacy or the plans themselves to confirm details. Sometimes small differences add up to big savings or hassles avoided.
You can explore the official list of Medicare-approved pharmacies and plan networks on Medicare.gov’s page about drug plan pharmacies. And if you want to dive deeper into how preferred pharmacy networks impact costs and choices, there’s a thoughtful analysis available on PubMed that breaks down the savings and switches these networks cause.
Remember, how to choose Medicare Part D prescription plan isn’t just about the plan on paper. It’s about making sure you can get your meds where it’s easiest and cheapest for you. That peace of mind? Totally worth the effort.

Step 5: Enroll Properly and Understand the Enrollment Periods
There’s nothing quite as frustrating as picking the right Medicare Part D plan, only to fumble the enrollment part. And trust me, missing your enrollment window can mean penalties or no coverage when you need it most. So let’s talk about enrolling properly and why timing is everything.
What Are Enrollment Periods Anyway?
Think of enrollment periods as the seasons when Medicare opens the doors for you to hop on or switch plans. Outside these windows? The doors might be closed tight, unless you’ve got a special circumstance.
The most crucial one is the Initial Enrollment Period. This starts 3 months before you turn 65, includes your birthday month, and lasts 3 months after. Twenty-four months of waiting? That could hit you with a late enrollment penalty that tweaks your premiums higher—and no one wants that surprise.
But it’s not just about joining. Open Enrollment (usually from October 15 to December 7 each year) lets you review and make changes for the coming year. If you missed your first chance or your needs shift, this is your opportunity.
Special Enrollment Periods: Life Happens
Lost coverage at work? Moved to a new area? These events might qualify you for a Special Enrollment Period (SEP). Giving you a window to enroll or switch plans outside the usual times.
Here’s a quick tip: Keep track of these dates—set reminders. It might feel like a hassle, but think about how peace of mind feels when you know you’re covered without surprise fees.
How to Enroll the Right Way?
Once you pick your plan, enrolling isn’t rocket science but skipping a step could backfire. You’ll typically enroll online via the Medicare website, by phone, or even with help through an agent (hello, expert guidance from Life Care Benefit Services if you want a hand).
Make sure you have your Medicare number handy (found on your card), personal details, and plan information. Double-check everything before submitting—typos can create delays or deny your enrollment.
Also, keep records of confirmation notices and communications. If there’s ever a hold-up or mix-up, having proof helps fast-track solutions.
Why Does This Matter?
Missing deadlines can add up to costly late enrollment penalties on your premiums—sometimes a 10% increase for every full year you delay enrollment without other credible coverage. Plus, there’s the risk of gaps in prescription drug coverage, which often translates to unexpected out-of-pocket expenses.
Does this really work? Yes. People who stay on top of enrollment periods usually avoid these penalties and get the best coverage to fit their changing needs.
Want a simple rule of thumb? Mark your calendar for your Initial Enrollment Period and Open Enrollment Period every year. Don’t wait for the last minute—plans can fill up, or you might miss out on your preferred coverage.
Remember, understanding how to choose Medicare Part D prescription plan means nothing if you don’t seal the deal by enrolling properly and on time. It’s that simple.
For more detailed guidance, check out Medicare’s official page on joining a Medicare drug plan and their tips on avoiding enrollment penalties. Staying informed can save you big headaches down the line.
And while we’re on the topic of timing, if you’re juggling other insurance needs, like navigating group health insurance options or comparing life insurance policies, give Life Care Benefit Services a shout. There’s a lot out there, but you don’t have to figure it all out alone.
Conclusion
Choosing the right Medicare Part D prescription plan isn’t just about saving a few bucks—it’s about peace of mind. You know that nagging worry about whether your meds will be covered or if unexpected costs will sneak up on you? Yeah, that’s exactly why staying on top of enrollment and understanding your options matters.
Remember, how to choose Medicare Part D prescription plan boils down to knowing your drugs, your budget, and the timelines you can’t miss. If you’ve felt overwhelmed before, you’re not alone. But here’s what I’ve learned: a little preparation goes a long way.
So, what’s your next move? Mark those enrollment dates on your calendar right now. Give yourself room to explore plans rather than scrambling at the last minute. And if you’re feeling stuck, Life Care Benefit Services is here—offering personalized help that doesn’t just push paperwork but actually fits your life.
Imagine sleeping easier knowing your prescriptions are covered without surprise charges. It’s not a pipe dream—it’s what smart planning gets you. So don’t wait. Reach out, get your questions answered, and take control. Because how to choose Medicare Part D prescription plan isn’t just a question—it’s a key step to safeguarding your health and wallet both.
Frequently Asked Questions (FAQ)
How soon should I sign up for Medicare Part D?
Honestly, timing can feel tricky. You want to avoid gaps in coverage, but don’t rush before knowing your options. The best move? Sign up during your Initial Enrollment Period, which starts three months before you turn 65 and lasts for seven months total. Missing that window can mean penalties or no coverage, so mark those dates and plan ahead.
Can I change my Medicare Part D plan once I enroll?
Good question. Yes, you can, but only during specific times like the Annual Election Period from October 15 to December 7. If you realize halfway through the year that your plan isn’t cutting it—maybe your meds aren’t covered or costs are higher than expected—this is your shot to switch. Outside these windows, changes are usually limited, so keep a close eye on your plan’s performance and pricing.
What if my medication list changes after I pick a plan?
Life throws curveballs, right? If your prescriptions change, you might be stuck with a plan that’s less ideal. That’s why shopping for a plan involves predicting your meds for the upcoming year as best as you can. If new meds come up, the Annual Election Period is your chance to adjust. It’s a bit of a balancing act, but staying flexible and informed helps you avoid surprise costs.
How do I know if a Medicare Part D plan covers my specific drugs?
This is a biggie. Every plan has a formulary—fancy word for their drug list. Before you commit, grab that list and compare it to your prescriptions. Don’t just look for your drug names; check the tier it’s on too because that affects your copay or coinsurance. Sometimes a similar alternative might be cheaper or more available. It takes a little homework, but it’s worth it for peace of mind.
Are there extra costs I need to watch out for with Medicare Part D?
Absolutely. Beyond the monthly premium, watch for deductibles, copays, coinsurance, and coverage gaps known as the “donut hole.” Costs can vary widely between plans, and what looks cheap upfront might cost you more later. A plan with a slightly higher premium but better overall savings on your meds might be smarter. That’s why it’s crucial to look at your actual drug expenses, not just the sticker price.
What if I miss the enrollment deadline?
Missing deadlines can happen, but it usually isn’t great news. You could face a late enrollment penalty, making your premiums higher permanently. However, if you have other credible prescription drug coverage, like through an employer, you might delay without penalty. If not, reach out for help ASAP—sometimes there are special enrollment periods if your situation changes. Don’t just assume it’s too late; there’s usually a way, even if it’s not obvious.
Where can I get help picking the right Medicare Part D plan?
Look, this stuff can feel overwhelming—that’s why you’re not alone. Independent agencies like Life Care Benefit Services exist to cut through the noise. They don’t just offer paperwork; they listen to your unique needs and help find plans that actually fit your life and budget. If you want peace of mind and fewer surprises, schedule a consultation now. Sometimes, a quick chat can save you hundreds or even thousands in the long run.
So, ready to take the next step? Questions answered and a clear path make how to choose Medicare Part D prescription plan not just doable, but smart planning.